Dementia & Alzheimer’s Disease Statistics and Facts (2024 Update)
Report Highlights:
- There are 10.7% or 6.5 million Americans (65 and over) living with Alzheimer’s in 2022 [4].
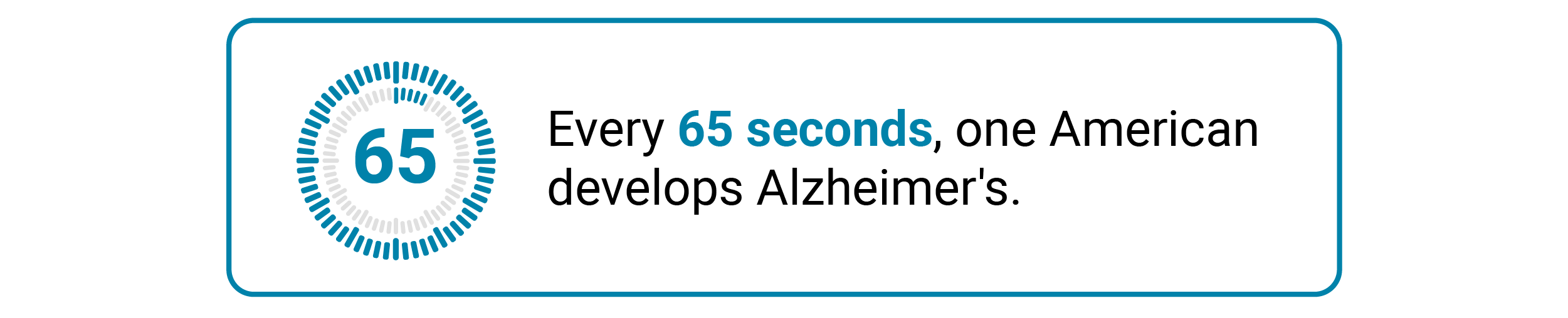
- Every 65 seconds, one person in the US develops Alzheimer’s disease [1].
- The number of individuals living with Alzheimer’s disease can increase to 13.8 million by 2060 [4].
- 4 million women (12%) and 2.5 million men (9%) have Alzheimer’s disease [4].
- 72.9% (4.72 million) of the total Alzheimer’s cases in the US are people aged 75 and above [4].
- California has the highest number of Alzheimer’s cases, with 690,000. The state also has the highest number of Alzheimer’s deaths, with 18,775 in 2020 [4] [10].
- Alzheimer’s disease is highest among Black Americans at 19% [4].
- Black Americans have a 1.5 to 2 times higher risk of Alzheimer’s, compared to White Americans [17].
- Daily racism increases the risk of developing poor cognition among African American women by 2.75 times. Daily institutional racism increases it by 2.66 times [11].
- Black Americans shell out 41% more than White Americans from the time of diagnosis to death [21].
- Life expectancy after Alzheimer’s diagnosis ranges from 3 to 11 years, with a median survival time of 8.3 years [7] [18].
- COVID-19 infection increases Alzheimer’s risk by 50% to 80%, especially in people aged 65 and older [29].
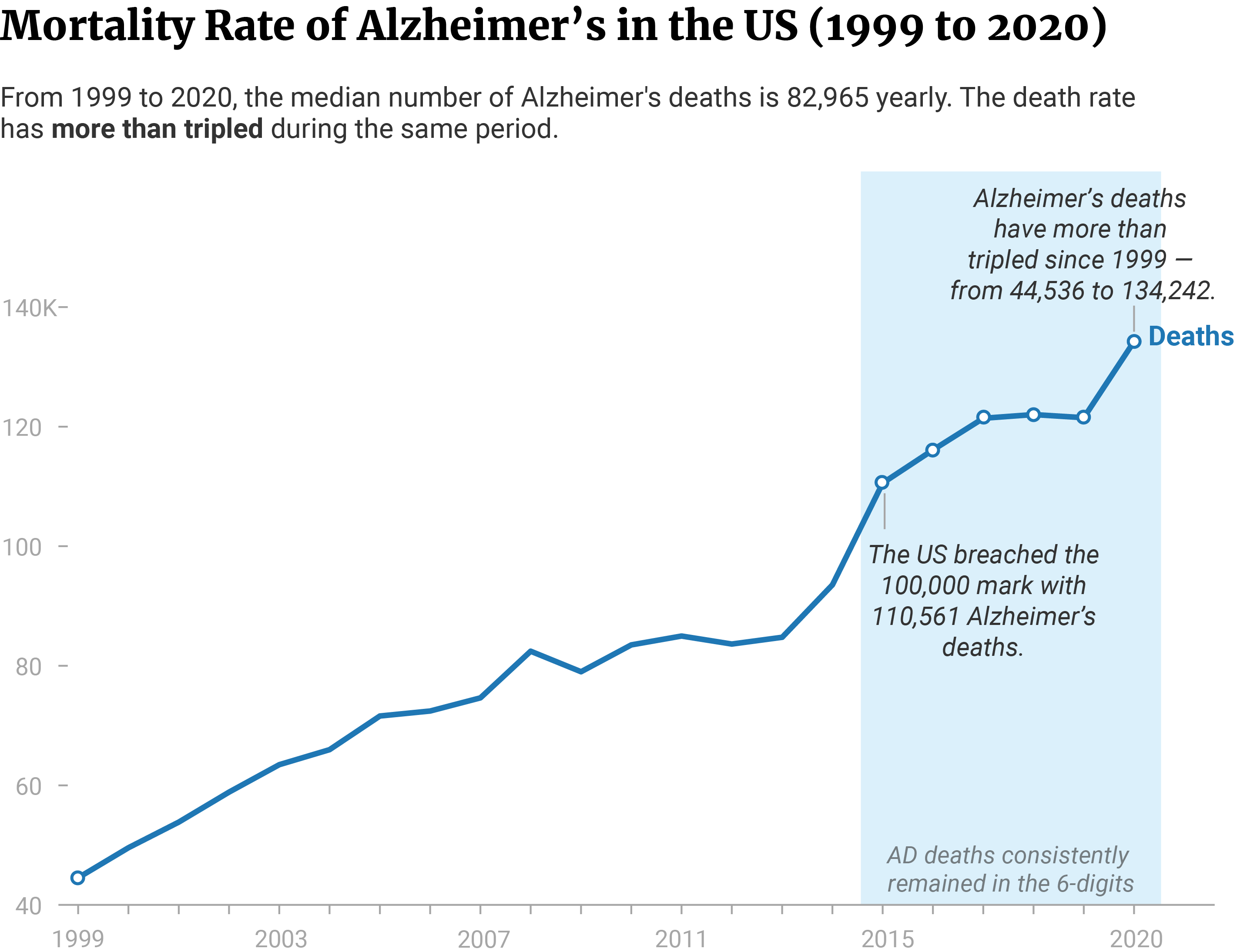
- 82,965 people die from Alzheimer’s and its complications each year [10].
- 12% to as high as 70% of dementia patients die from pneumonia [19].
- The cost of Alzheimer’s disease in the US will amount to $321 billion by the end of 2022 [4].
It’s normal to experience some memory changes as you grow older. But if it starts affecting your day-to-day activities, it may be a sign of dementia.
Dementia isn’t a disease. It’s a symptom of brain disorders that affect cognitive function, and the primary contributing factor is Alzheimer’s disease.
According to the WHO, 60% to 70% of people with dementia have Alzheimer’s disease [12]. It’s the leading cause of dementia among older people. It also contributes to an elderly’s disabilities and dependence on another person.

Other brain disorders that cause dementia include Parkinson’s disease, severe head injuries, and Creutzfeldt-Jakob disease. These cause brain degeneration that impairs cognitive function.
Blood vessel problems like heart disease and stroke also contribute to dementia development. Both heart disease and stroke damage the brain’s blood vessels and lead to vascular dementia. Vascular dementia accounts for 15% to 20% of all dementia cases [14].
Read on and learn more about the current Alzheimer’s disease facts and statistics in the US.
What is Alzheimer’s Disease?
Alzheimer’s disease is a neurodegenerative disease characterized by irreversible neuronal loss. It’s caused by the accumulation of tau proteins and neurofibrillary tangles in the brain tissue. It damages the neurons and results in progressive dementia and memory loss.
As the disease progresses, the brain loses more of its cognitive ability. It affects communication, memory, language, and motor functions. It also affects how one responds to and interacts with their environment.
Alzheimer’s is a debilitating disease that interferes with one’s daily life. It eventually forces patients to depend on caretakers.
What are the Most Common Causes of Alzheimer’s Disease?
A family history of this disease gives you a 70% risk of developing Alzheimer’s disease. 30% of the risk can come from environmental factors. These include exposure to hazardous compounds, pollutants, and chronic health problems [30].

The APOE-e4 gene, in particular, plays a crucial role in the development of Alzheimer’s disease.
56% of Americans diagnosed with Alzheimer’s disease had at least one copy of the APOE-e4 gene. 11% had two copies of the gene [4].
The presence of one APOE-e4 copy increases Alzheimer’s risk by 3 times. The risk further increases by 8 to 12 times in those with two APOE-e4 copies [4].
Age also increases Alzheimer’s risk. The older you get, the higher the risk. However, it should be noted that Alzheimer’s disease isn’t a normal part of the aging process. Instead, it’s a chronic, progressive disease.
33.2% of people aged 85 and older have Alzheimer’s disease, compared to 5% of those between 65 and 74 years [4].

Smoking contributes to the development of Alzheimer’s as well. It causes cellular inflammation and worsens several health factors that increase Alzheimer’s risk. These include heart diseases, obesity, diabetes, hypertension, and hypercholesterolemia [8].
- Current smokers have a 79% higher risk of developing Alzheimer’s than never-smokers.
- Ever-smokers carry a 21% higher risk, compared to never-smokers.
- Former smokers also have a 1% higher risk of having Alzheimer’s, compared to never-smokers.
- Current smokers have a 70% higher Alzheimer’s risk, compared to former smokers.
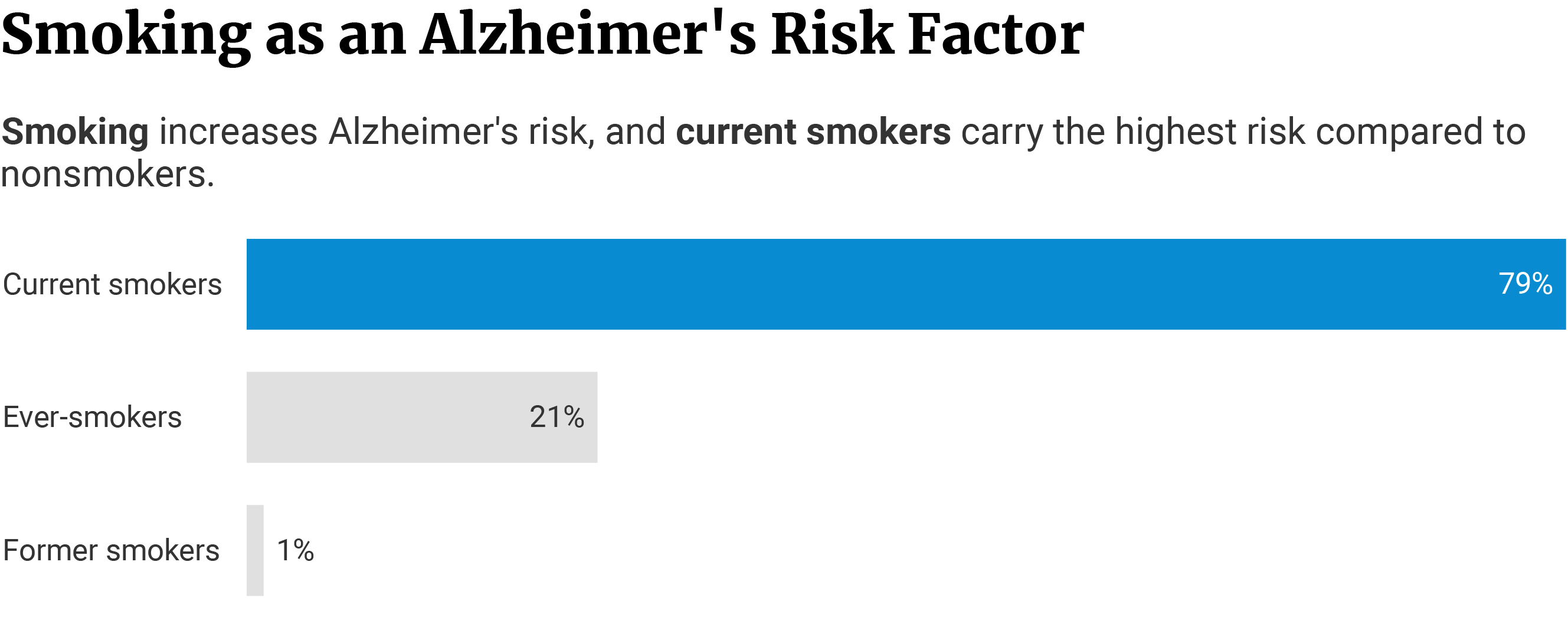
A study also found dementia risk is higher among smokers by 45% than among nonsmokers [24].
It also noted that smoking may have potentially contributed to 14% of the world’s Alzheimer’s cases [24].
How Many Stages Are There in Alzheimer’s Disease?
Alzheimer’s disease has 7 stages [2].
Stage 1: No dementia seen
This early stage is still free from noticeable dementia symptoms. However, dementia may have already started years before.
Some memory loss is present. However, the person often associates it with the normal aging process. They don’t usually see it as one of the first symptoms of Alzheimer’s and other forms of dementia.
Stage 3: Mild cognitive impairment
The person now has some problems with focus, concentration, and memory. Their comprehension skills may also show some impairment.
The warning signs of the disease are now more noticeable to others as well.
Stage 4: Moderate cognitive impairment (mild dementia)
The cognitive decline is now much more noticeable and starts to affect day-to-day life. Dementia symptoms also become more pronounced.
Stage 5: Moderately-severe cognitive impairment (moderate dementia)
The person now needs assistance as they are unable to live on their own. They also start having problems recalling familiar information. These include the names and their relationships with other people.
Stage 6: Severe cognitive impairment (moderately-severe dementia)
The person becomes more dependent on their caretaker. They may need help with eating, bathing, grooming, and dressing.
Dementia symptoms have also gotten worse. They may forget family members’ names, including their spouses and children.
The person also exhibits changes in emotions, moods, and personality.
Stage 7: Very severe cognitive decline (severe dementia)
In the end stage, the patient is now dependent on their caretaker for all activities of daily living.
Communication and language skills have also severely declined. Under stage 7a, speech is limited to half a dozen words or fewer. Under 7b, the patient loses his ability to speak.
As the disease progresses further, it begins to affect motor skills and ambulation. In 7c and 7d, the patient loses the ability to walk and sit independently. By stage 7e, the patient loses his ability to smile.
In the last stage (7f), the patient can no longer hold his head up on his own.
Alzheimer’s Prevalence in the US
2022 data shows that Alzheimer’s disease has an annual prevalence of 10.7%. It affects older adults 65 and older [4].
It has a lifetime prevalence of 58 million in 2021. This figure may increase to as high as 88 million by 2050, a 51.72% increase in about three decades [4].
How Many People Have Alzheimer’s Disease?
Alzheimer’s disease affects 6.5 million (nearly 1 in 9) Americans age 65 and older [4].
![]()
The disease affected 6.2 million Americans in 2021 [3]. Trends show that it can increase by nearly half a million new cases this year. This means that, for every 65 seconds, one person in the US developed Alzheimer’s disease [1].
By 2025, Alzheimer’s disease will affect 7.2 million older Americans, an increase of 10.77% in less than 5 years. It’s also projected that 12.7 million older Americans will develop the disease by 2050 [4].
If this trend continues, we’ll see the cases more than doubling to 13.8 million by 2060 [4]. That’s a 112.31% increase or 7.3 million new cases from 2022 to 2060.
The number of global Alzheimer’s disease cases is currently at 55 million, says the WHO [12].
It’s the 7th leading cause of death across the globe [13].
Without medical breakthroughs, we’ll see an estimated 10 million new cases yearly [12]. That’s one person in the world developing Alzheimer’s every 3.2 seconds.
The global number seems to be just the tip of the iceberg. According to the 2022 World Alzheimer Report by Alzheimer’s Disease International, 75% of the global dementia cases remain undiagnosed [15].

Alzheimer’s Prevalence by State
Owing to their large populations, California has the highest number of Alzheimer’s patients, with 690,000 in 2020. Florida follows in second place, with 580,000 and New York in third place, with 410,000 [4].
The state with the lowest number of Alzheimer’s patients is Alaska, with 8,500. Wyoming, with 10,000, and Vermont, with 13,000 follow [4].
Based on crude rate, Florida has the highest Alzheimer’s rate, with 2.67% of its population living with the disease. Rhode Island ranks second at 2.27% and Connecticut at third, with 2.25% [4].
States with the lowest Alzheimer’s rates are Utah at 1.05%, Alaska at 1.16%, and Colorado at 1.31% [4].
By 2025, California’s prevalence will increase to 840,000, Florida, with 720,000, and New York, with 460,000 [4].
Alaska’s Alzheimer’s disease cases will also increase to 11,000 by 2025. Wyoming’s will go up to 13,000 cases and Vermont’s to 17,000 [4].
Arizona will have the highest percentage increase of 33.3% — from 150,000 in 2020 to 200,000 in 2025 [4].
Vermont comes second, with a 30.8% percent increase. Nevada’s cases will increase by 30.6% — from 49,000 in 2020 to 64,000 in 2025 [4].

Factors that influence the prevalence of Alzheimer’s disease in each state:
- Geography and the presence of environmental risk factors such as selenium levels in the soil
- Population and demographics
- Cultural and inter-regional differences
- Stigma
- Awareness and understanding of the disease and its symptoms
- Access to medical care
- Diagnostic practices
- Quality of medical care
- Prevalence of risk factor diseases
Alzheimer’s Statistics and Demographics in the US
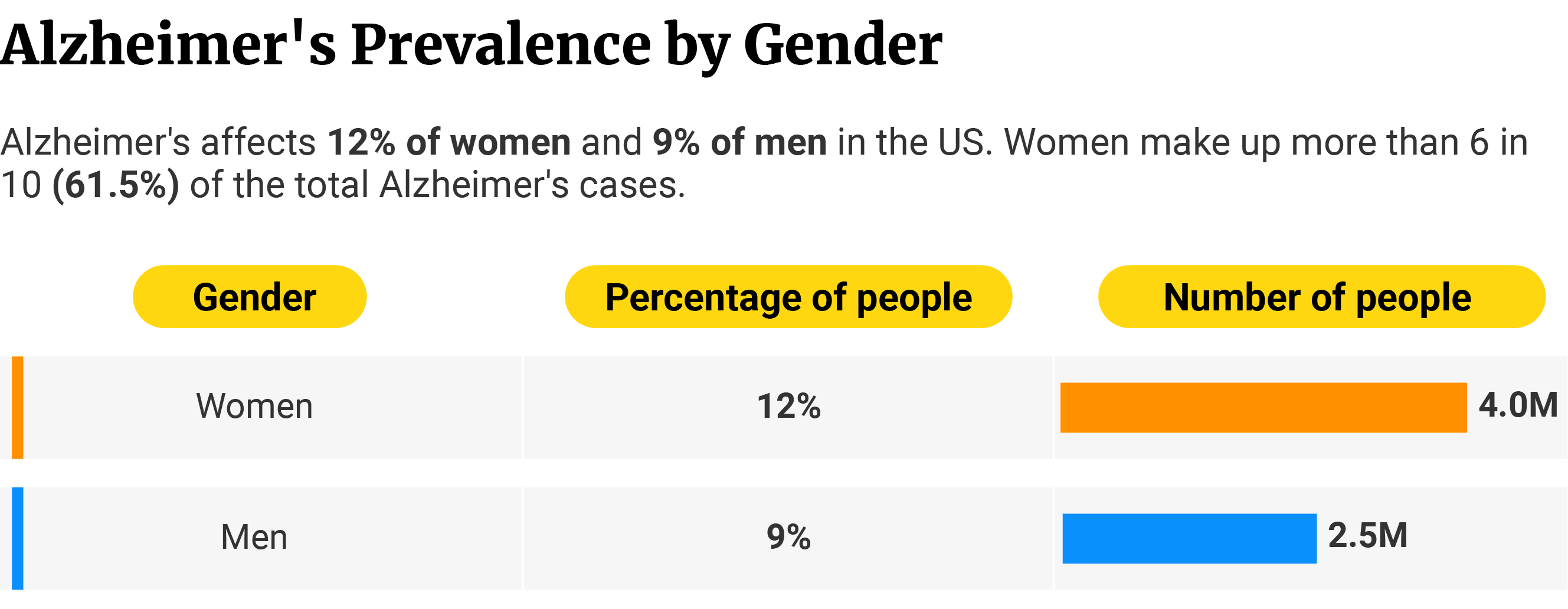
Alzheimer’s disease is more prevalent in women at 12%, older people (75 to 84 years of age) at 37.2%, and Black Americans at 19%.
Alzheimer’s Disease Statistics: Male vs Female
12% or 4 million women (65 and older) in the US have Alzheimer’s disease [4].
This neurological disease affects women the most. They make up more than 6 in 10 of those with Alzheimer’s [4].
It affects men the least. Compared to women, only 9% or 2.5 million men have Alzheimer’s disease [4].
According to the Alzheimer’s Association, factors that influence the prevalence rates include:
- Biological factors
- Sociocultural factors
- Socioeconomic factors
- Presence and prevalence of risk factor diseases
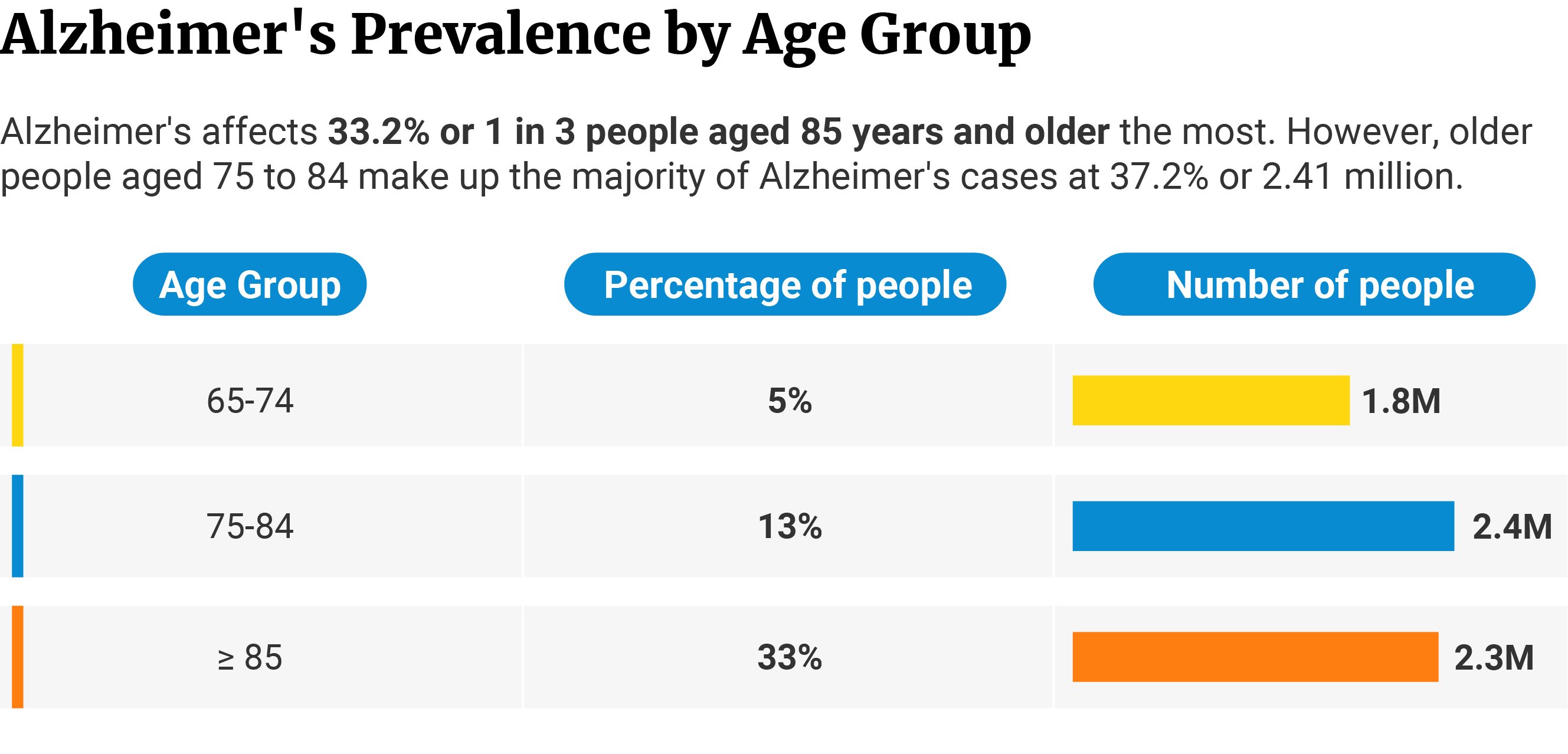
Alzheimer’s Disease Statistics: Age Group
33.2% of people 85 years and older have Alzheimer’s. They’re the age group most vulnerable to the disease. They make up 35.7% of the total number of people with Alzheimer’s, with the disease affecting 2.31 million of their population [4].
Alzheimer’s affects those who belong to the 65-to-74-year age group the least. 5% of their population have Alzheimer’s. It affects 1.75 million people, and they make up 27% of the total Alzheimer’s cases [4].
Alzheimer’s affects 13.1% of people between 75 and 84 years of age. They make up the majority of Alzheimer’s cases at 37.2% with 2.41 million people [4].
Of the 6.5 million people with Alzheimer’s disease, 72.9% of them are 75 years of age or older [4].
What‘s the Average Age of Alzheimer’s Onset?
The first signs of Alzheimer’s disease typically show up when a person is in their mid-60s [20]. Called late-onset Alzheimer’s disease, it’s the most common form.
Symptoms can also appear when a person is in their 30s to mid-60s [20]. Called early-onset Alzheimer’s disease, this type is rarer compared to the former.
Alzheimer’s Disease Statistics: Race
Alzheimer’s affects Black Americans the most, with 18.6% of those aged 65 and older having this disease. The disease affects 1.06 million of this population [22].
Hispanic Americans follow in second place. It affects 14.0% of their population or 0.71 million people [22].
Alzheimer’s disease affects non-Hispanic White Americans the least. Compared to other ethnicities, this disease only affects 10.0% of their population. However, they make up the bulk of Alzheimer’s cases at 70.8%, with 4.3 million of their population suffering from the disease [22].
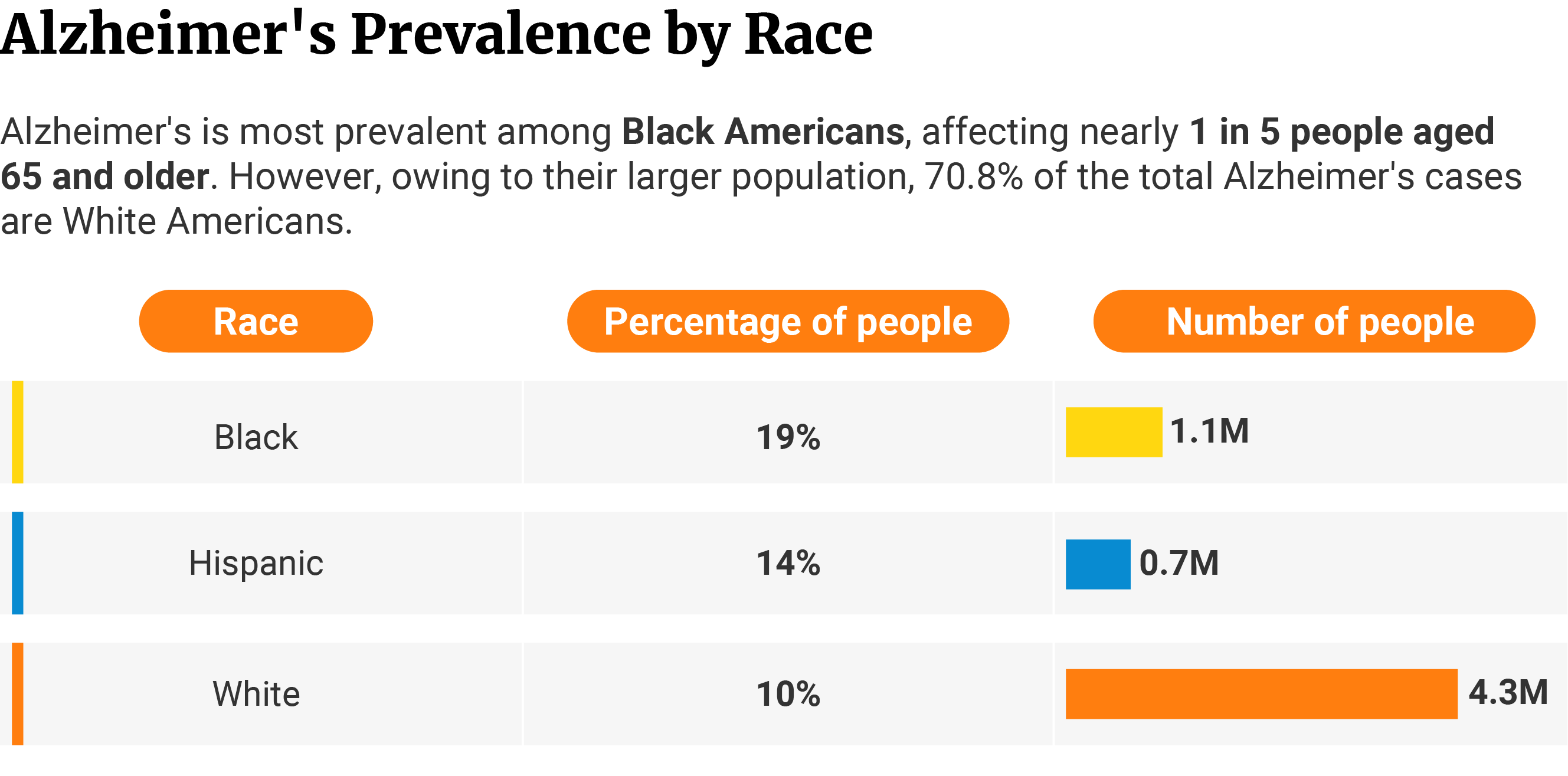
Black Americans have the highest likelihood of developing Alzheimer’s disease. They carry more Alzheimer’s risk factors. They also develop more severe symptoms and cognitive impairments.
Older Black Americans are 1.5 to 2 times more likely to develop Alzheimer’s and related dementias than Whites. They’re also 2 times more likely to develop hallucinations and delusions [17].
![]()
But despite these national statistics, studies say they’re 35% less likely than non-Hispanic Whites to be diagnosed with Alzheimer’s disease [17].
Social attitudes and racial discrimination may have something to do with the disparity.
The Alzheimer’s Disease Research Centers (ADRCs) studied 15 years of data from 2005 to 2020. It comprised 5,700 Black Americans and 31,225 White Americans. They found that only 26.8% of Black Americans were diagnosed with Alzheimer’s at their baseline visit. Early diagnosis at baseline visit was higher among White Americans at 36.1% [17].
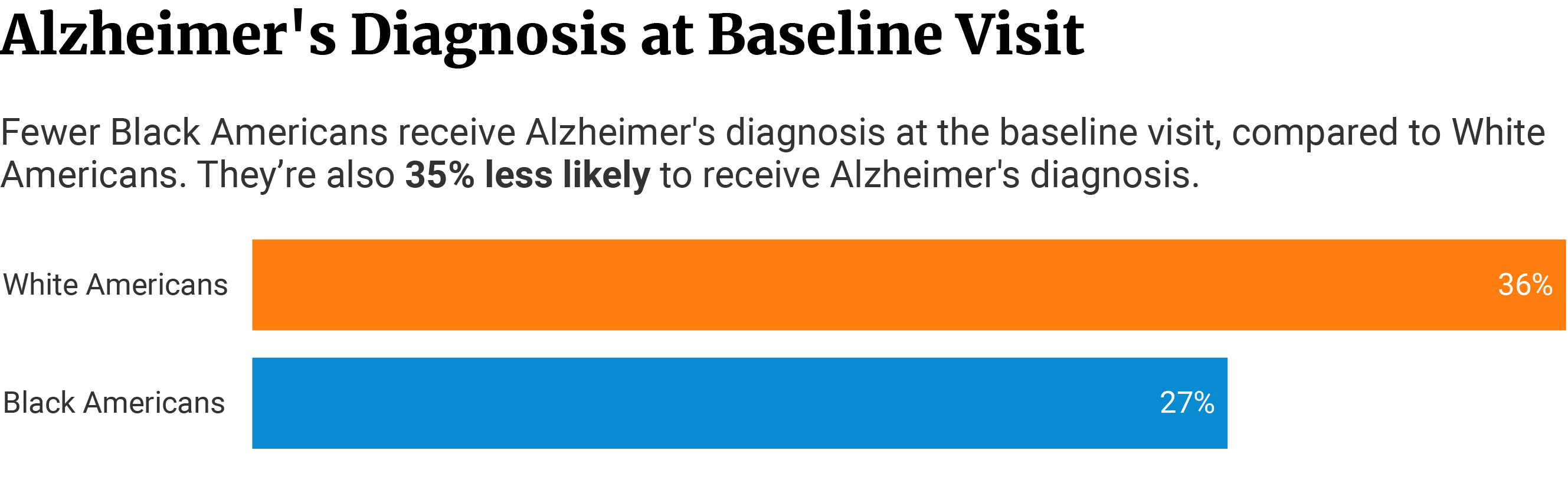
Researchers also found that Black Americans have 35% lower odds of being diagnosed with Alzheimer’s disease, despite having higher risks and more severe symptoms and cognitive impairments [17].
One reason for this is social beliefs among Black Americans. Older Black Americans often seek treatment when other neuropsychiatric symptoms begin showing up. Memory loss, as a symptom of Alzheimer’s or other dementias, is often ignored. They often consider memory problems a common sign of normal aging [17].
Healthcare discrimination also plays a significant role in the disparity. Compared to White Americans, Black Americans often have to show more severe clinical symptoms before physicians consider a dementia diagnosis. This means they get diagnosed when their Alzheimer’s has become more advanced [17].
Delayed diagnosis due to racial discrimination increases the prevalence rate among Black Americans. It also prevents them from receiving early intervention.
Racial Discrimination in Alzheimer’s Disease Health Care
50% or 1 in 2 Black Americans report feeling high levels of discrimination when seeking help [5].
We can observe the same trend among other ethnicities.
42% or more than 2 in 5 Native Americans feel discriminated against [5].
1 in 3 Asian Americans (34%) and Hispanic Americans (33%) also report a higher rate of racial discrimination [5].
Among non-Hispanic White Americans, only 9% of them report healthcare inequity [5].

It’s not just the patients who report discrimination but their caregivers as well. They feel that, because of their color and race, healthcare providers don’t listen to them.
Again, this perception appears highest among Black Americans. 42% or more than 2 in 5 Black caregivers report discrimination, compared to 17% or about 1 in 6 White caregivers [5].
Racial discrimination is also higher among other non-White caregivers.
Fewer than 1 in 3 Native Americans (31%) and Asian American (30%) caregivers also report the same [5].
Among Hispanic caregivers, more than 1 in 4 (28%) say they feel discriminated against as they navigate around the healthcare settings for their patients [5].
Caregivers identifying with minority groups or ethnicities also reported high levels of other forms of discrimination [5]:
- 43% of native American caregivers say they’ve been made to feel not smart, compared to 11% of White Americans. 28% of Asians and 28% of Black Americans experience the same.
- 26% of Black and 26% of Hispanic American caregivers say they’re treated with less courtesy. Among White Americans, only 11% report the same.
- 27% of Native and 26% of Black American caregivers say they’re treated with less respect. Only 8% of White Americans experience the same.
- 21% of Hispanics and 19% of Black Americans receive poor medical attention and care. Only 7% of White Americans report the same incident.
- 13% of Black Americans say the providers acted afraid of them, compared to 7% of White Americans.

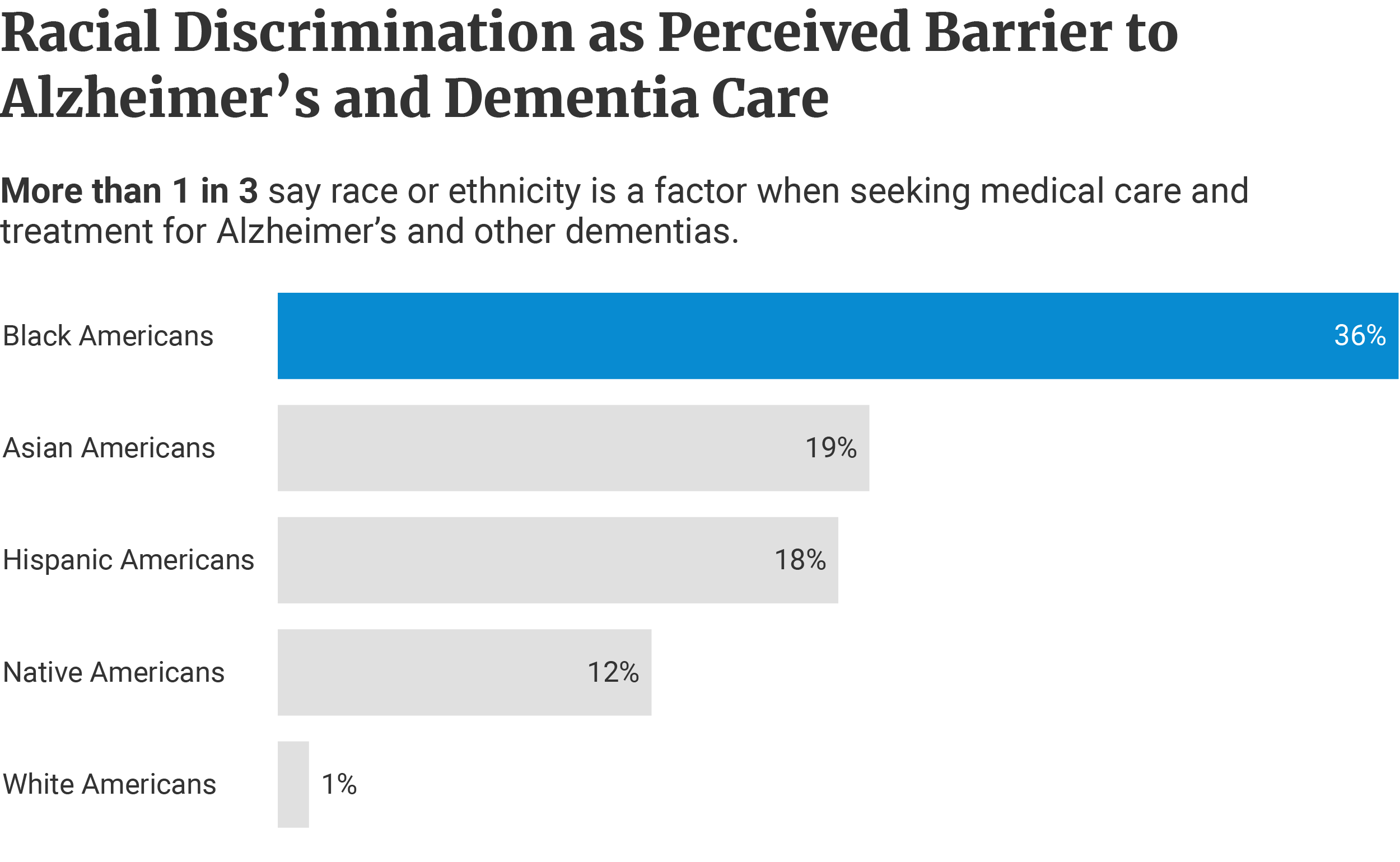
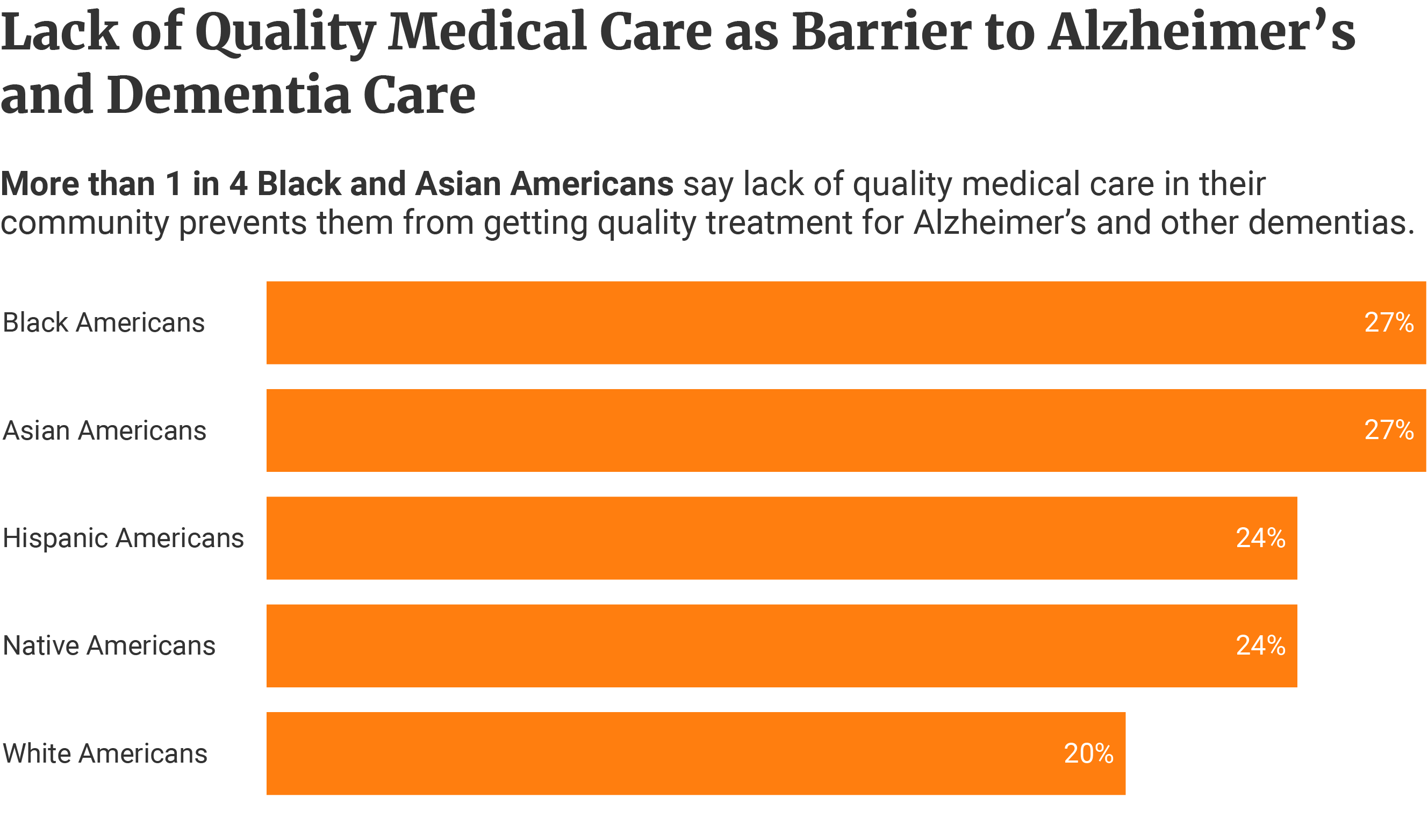
Perceived Barriers to Dementia and Alzheimer’s Disease Care
36% or 1 in 3 Black Americans say discrimination is a barrier to getting prompt medical care for Alzheimer’s [5].
Nearly 1 in 5 Hispanic Americans (18%) and Asian Americans (19%) also say the same. 1 in 8 or 12% of Native Americans also agree [5].
Only 1% of White Americans say discrimination is a barrier to receiving medical care [5].
Lack of quality medical care in their communities is also an issue. This perception appears highest among Black and Asian Americans at 27% each [5].
24% of Hispanic Americans and 24% of Native Americans share the same views [5].
Among White Americans, only 20% say lack of quality healthcare is an issue [5].
Effects of Racism on the Brain’s Cognitive Health
High levels of daily racism put African American women at 2.75 times higher risk of developing poor cognition [11].
High levels of institutional racism increase the risk by 2.66 times more than those who aren’t exposed to racism [11].
![]()
Racism, the 2020 study found, negatively impacts the brain’s cognitive health. It also cited depression and insomnia as mediating factors [11].
What is the Average Life Expectancy of Someone Diagnosed with Alzheimer’s Disease?
From the time of diagnosis, people with Alzheimer’s disease usually have about 3 to 11 years to live. However, it’s also possible for some people with Alzheimer’s to live beyond 20 years from diagnosis [7].
Alzheimer’s disease is more commonly diagnosed during stage 4. It’s the stage when the patient begins to show mild dementia symptoms [7].
However, the disease process has already started 15 or more years earlier. It started before the patient even began exhibiting noticeable Alzheimer’s symptoms [1].
How Long Does It Take for Alzheimer’s to Progress?
Within a 5- to 10-year period, about 30% to 50% of people diagnosed with mild cognitive impairments due to Alzheimer’s disease progress to Alzheimer’s dementia [4].
How fast Alzheimer’s progress varies. Once mild cognitive impairments begin to show, the duration between each stage shortens.
Symptoms of mild cognitive impairment begin showing up at stage 3. This stage usually lasts 7 years. By the 4th stage, mild dementia symptoms appear [1].
The patient usually has about 6 years before cognitive impairment and dementia symptoms worsen and progress to stage 7 [1].
The seventh stage can last for about seven years [1] [2]:
- 7a: 1 year
- 7b: 1.5 years
- 7c: 1 year
- 7d: 1 year
- 7e: 1.5 years
- 7f: Indefinite
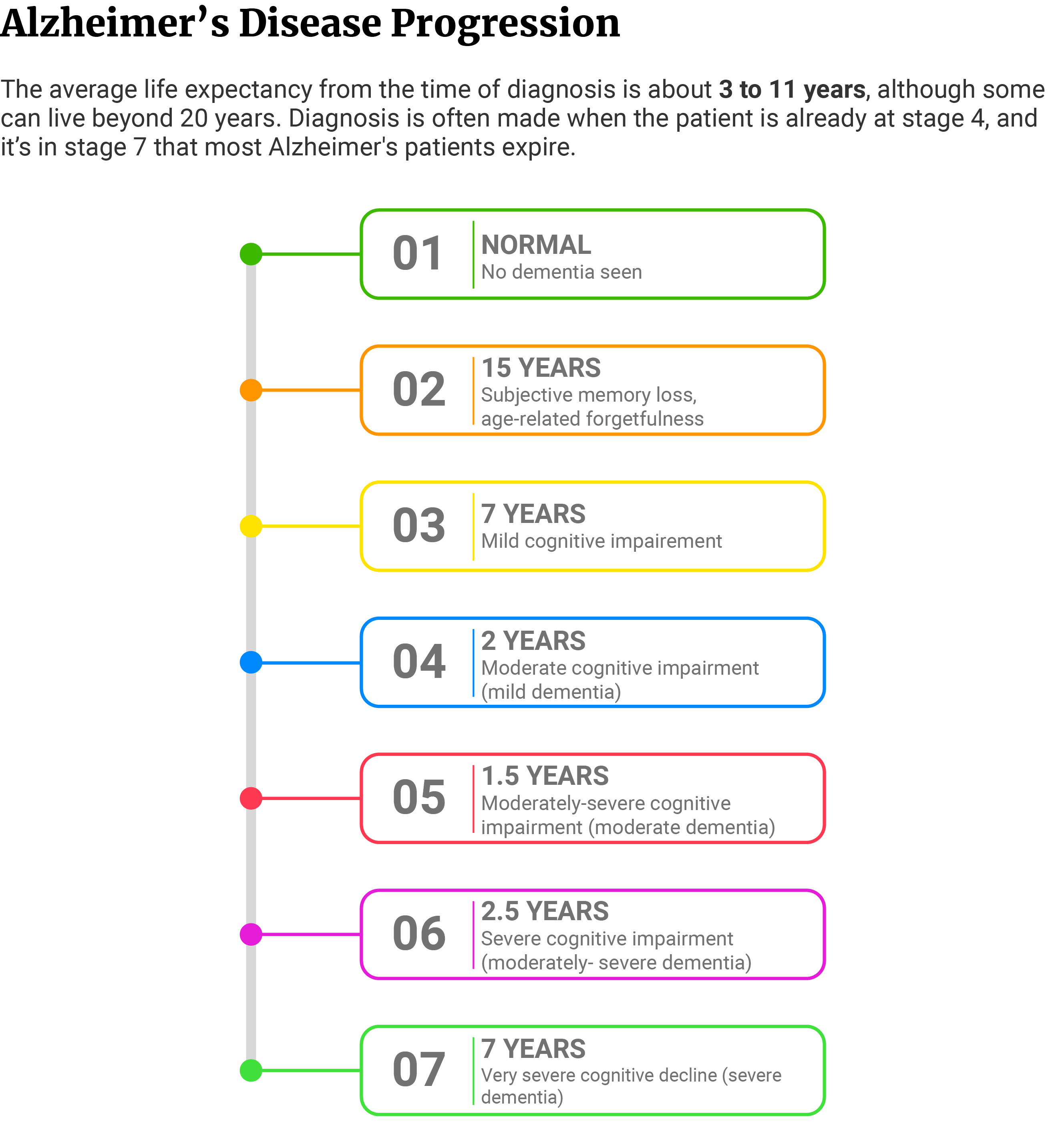
Most people with Alzheimer’s usually die at various stages during stage 7. The common causes of death include pneumonia and infected bed sores [2].
Life Expectancy Living With and Without Dementia
People with dementia have a shorter life expectancy than people without dementia.
A study followed 3,605 people aged 65 and older from 1994 to 2008. All participants had no dementia at the time of enrollment. However, the incidence of dementia increased as the participants aged. Between 85 and 89 years of age, the incidence was at 74.2 cases per 1,000 person-years and 105 cases per 1,000 person-years at 90 years and older [28].
The average life expectancy of a person decreases as one ages. However, the researchers noted that those living with dementia have a shorter life expectancy than those living without.
People without dementia who reached 70 years of age can expect an average life expectancy of at least 15.1 more years. This drops by 86.76% in people living with dementia who reached the same age. Their average life expectancy decreases to 2 years [28].
- Living with dementia at 70 years reduces life expectancy in women to 2.3 years and men to 1.7 years.
- Of those without dementia, the average life expectancy is 15.7 years in women and 14.3 years in men.
- The average life expectancy in men and women with dementia decreases by 85.35% and 88.11%, respectively.
People without dementia who reached 90 years can expect an average of 4.2 more years of life. On the other hand, people living with dementia who reached the same age have a shorter life expectancy of 1.3 years. Alzheimer’s disease reduces normal life expectancy by 69.05% [28].
- Women and men living with dementia at 90 years can expect an average of 1.5 and 1-year life expectancies.
- Women and men without dementia of the same age can expect an average of 4.5 years and 3.5 years, respectively.
- Life expectancy at this age decreases by 66.67% in women and 71.43% in men diagnosed with dementia.
Women with dementia live about half a year longer than men with dementia [28].
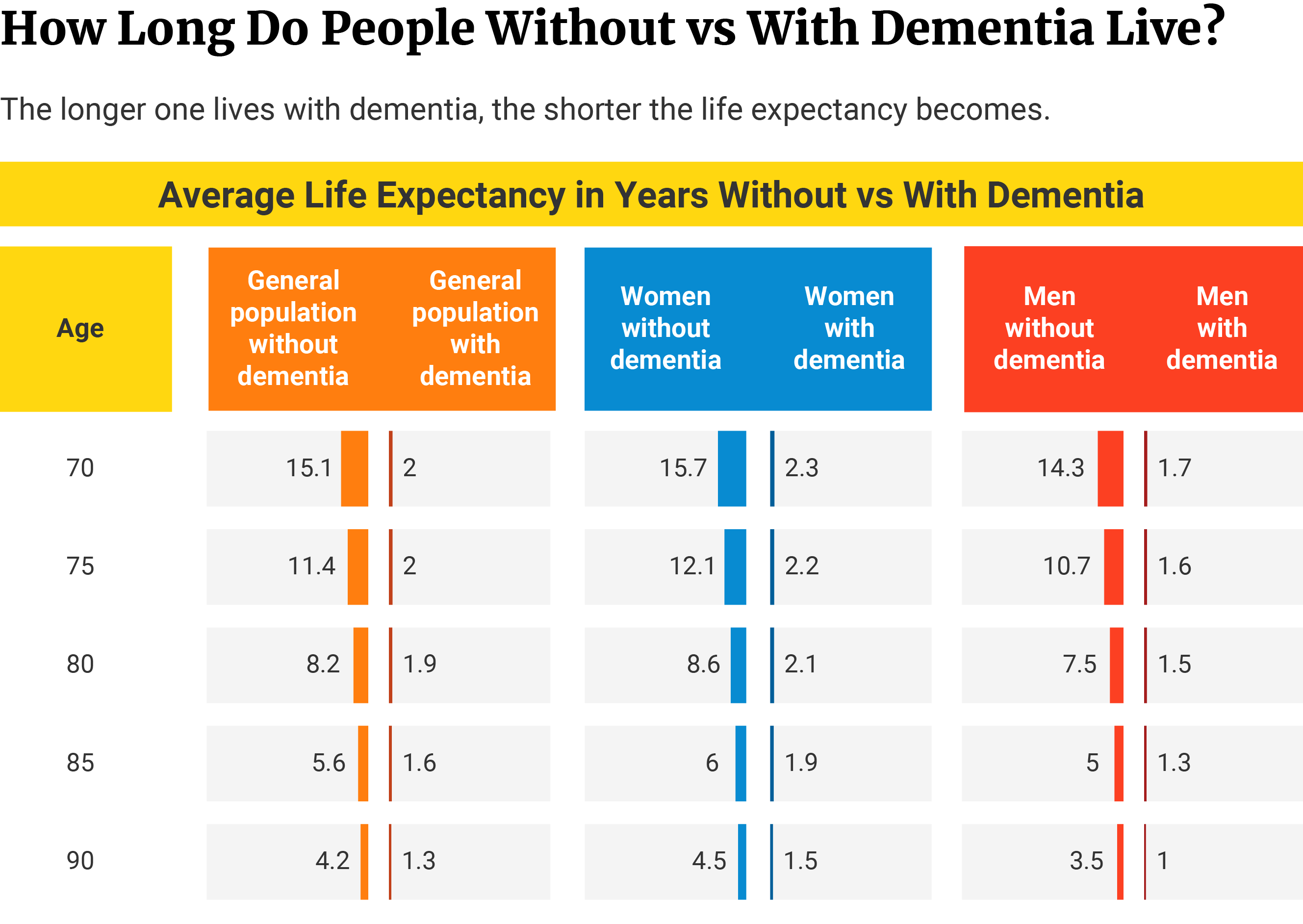
Note: The average life expectancies in the study are estimates based on Markov model, not clinical findings. This method estimates the average number of years a person with or without dementia is expected to live when reaching a certain age.
Survival Rate of Alzheimer’s Disease
Alzheimer’s disease diagnosed at the age of 65 has a median survival time of 8.3 years. It’s a 67% decrease in life expectancy compared to people of the same age without the disease [18].
A diagnosis at 90 years of age reduces survival time by 39%. Alzheimer’s diagnosis at this age gives the patient only about 3.4 years to survive [18].
The older one is at the time of the diagnosis, the shorter their survival time.
COVID-19 and Alzheimer’s Disease Statistics
Patients with Alzheimer’s have 20% higher odds of dying from COVID-19 than patients without it [31].
A recent study also showed that COVID-19 infection increases the risk of developing Alzheimer’s disease by 50% to 80% within a year after the infection [29]. The risk is highest among women and people aged 65 and older.
The data came from a study comprised of 6,245,282 older adults (65 and over) who had medical care during the pandemic. The date of study spanned from February 2020 to May 2021).
Alzheimer’s Mortality Rate and Statistics
The number of Alzheimer’s deaths has more than tripled — from 44,536 deaths in 1999 to 134,242 in 2020 [10].
It’s the 5th leading cause of death among older people 65 years and above. It’s the 7th leading cause of death in the country [10].
The risk of death in people with Alzheimer’s increases with age, compared to those without.
People at 70 years of age with Alzheimer’s have a 2 times higher risk of dying before they turn 80 [6].
People over 85 years have a 5 times higher risk of dying from this Alzheimer’s, compared to those aged 75 to 84 [26].
They also have a 50 times higher risk of dying from Alzheimer’s disease, compared to those who are aged 65 to 74 [26].
How Many People Die from Alzheimer’s Disease?
According to the CDC, 134,242 patients died from Alzheimer’s disease in 2020 [10].
From 1999 to 2020, a total of 1.87 million people succumbed to complications of Alzheimer’s disease. The median number of Alzheimer’s deaths amounts to 82,965 people each year [10].
In 2015, the US breached its 100,000 mark in Alzheimer’s deaths with 110,561. It’s also the year with the highest increase in Alzheimer’s death rate. 2015 showed an 18.2% or 17,020 increase from the previous year’s (2014) 93,541 [10].
2020 is the second deadliest year for Alzheimer’s patients. With 134,242 deaths, it’s a 10.49% or 12,743 increase from 2019’s 121,499 [10].
What’s the Average Age of Alzheimer’s Death?
The median age of death in 2020 is 79 [10]. Data is based on 2020’s death rate per single-year age. It included only the ages that had more than 100 deaths, starting at age 58.
We see almost the same trend in CDC’s 1999-2020 report.
Starting at 58 years, death rates per single-year age exceeded 1,000 deaths. The median age of death from 1999 to 2020 was also 79 [10].
What’s the Most Common Cause of Death in Alzheimer’s Patients?
Pneumonia-associated death occurred in 12% to 70% of patients with Alzheimer’s and other dementias [19]. It’s the leading cause of death among Alzheimer’s patients.
Studies show that patients with dementia have 2 times or 200% higher risk of dying from pneumonia, compared to those with no dementia [19].
Alzheimer’s Deaths Demographics and Statistics
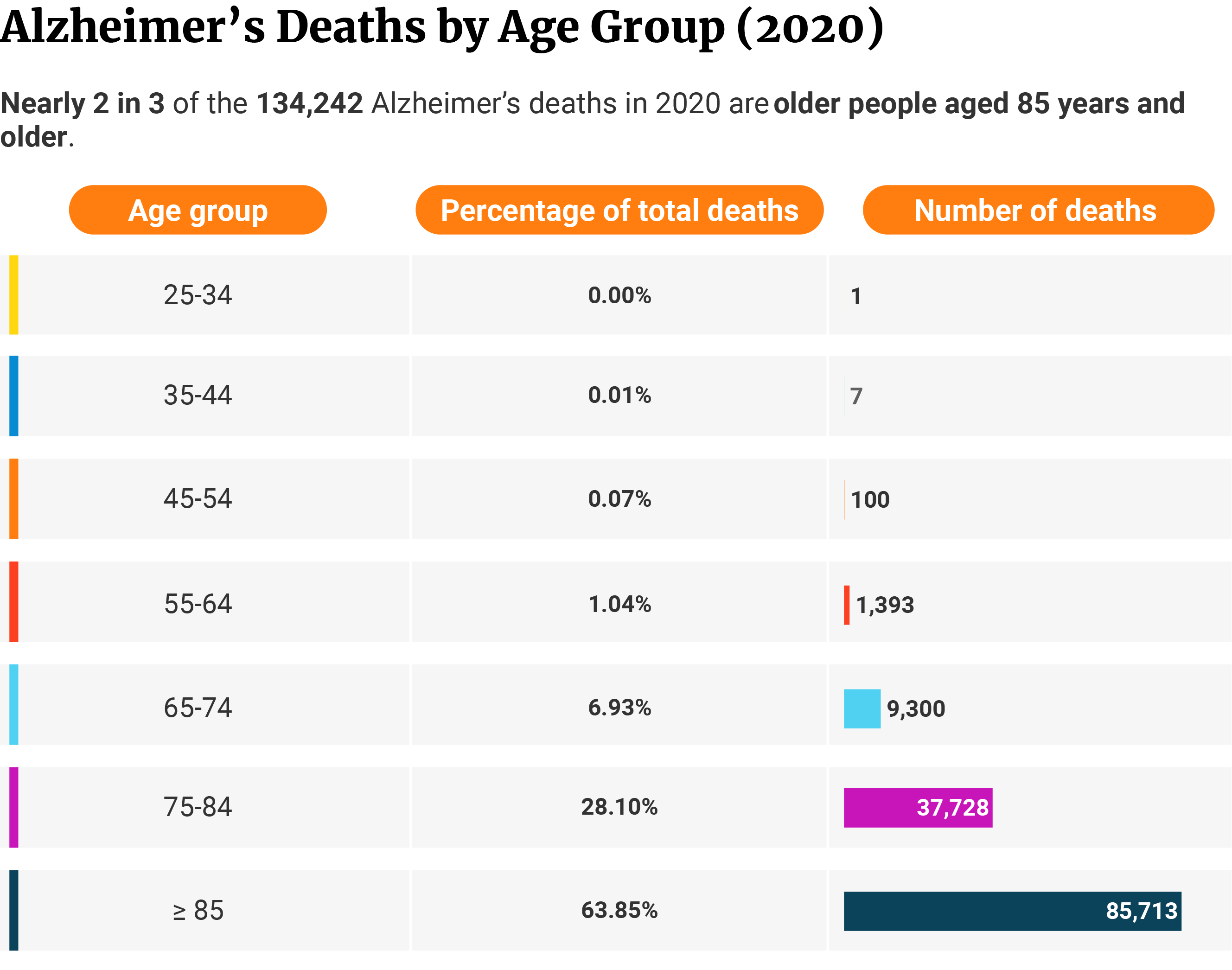
More than 2 in 3 Alzheimer’s deaths are women. More than 4 in 5 Alzheimer’s deaths are White Americans. Nearly 2 in 3 deaths are older people aged 85 and over.
Alzheimer’s Death Male vs Female Statistics
Of the 134,242 deaths in 2020, women make up 69.3% or 92,969 of the cases. Men make up 30.7% or 41,273 of the cases [10].
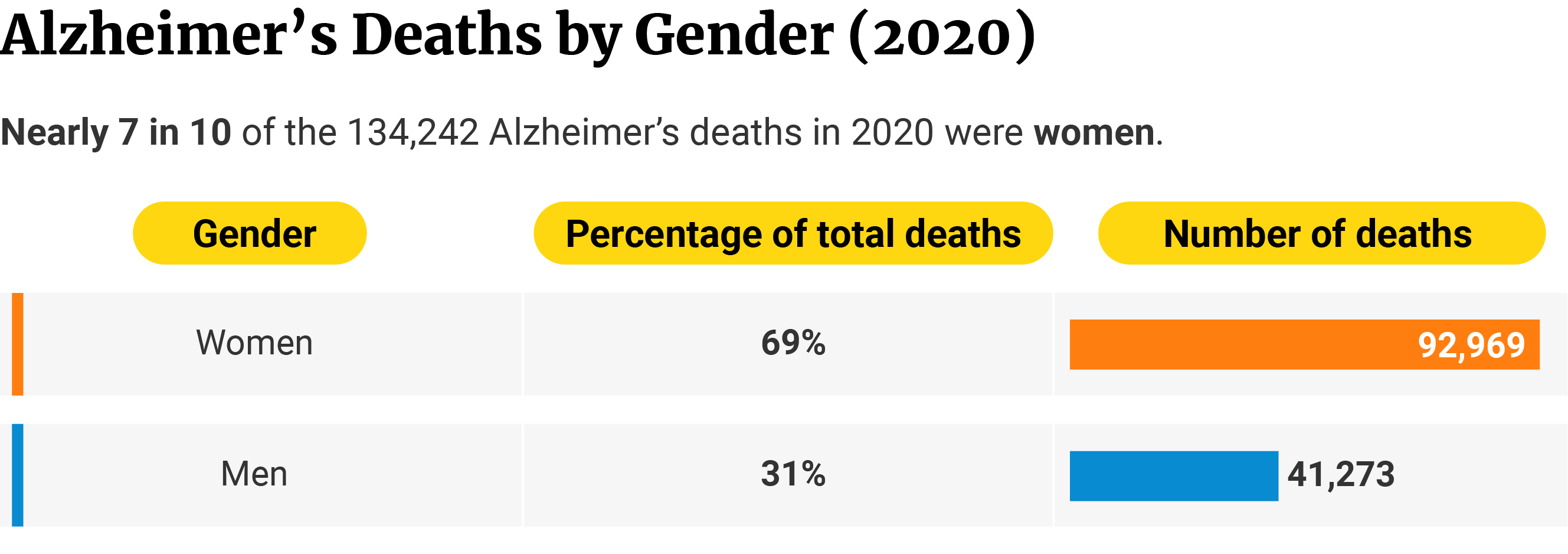
Women with Alzheimer’s disease have a 30% higher risk of dying than men [26].
Alzheimer’s Death by Age Statistics
Of the 134,242 deaths in 2020, 63.8% or 85,713 of them are 85 years and older [10].
The older the age, the higher the mortality risk.
28.1% or 37,728 deaths belong to the 75 to 84 age group, while 6.9% or 9,300 deaths belong to the 65 to 74 age group [10].
1% or 1,393 deaths occurred among the age group 55 to 64 years [10].
The age group 45 to 54 years had 100 deaths or 0.1% or 100 deaths [10].
Seven people died from the 35-to-44 age group, and one from the 25-to 34-age group [10].
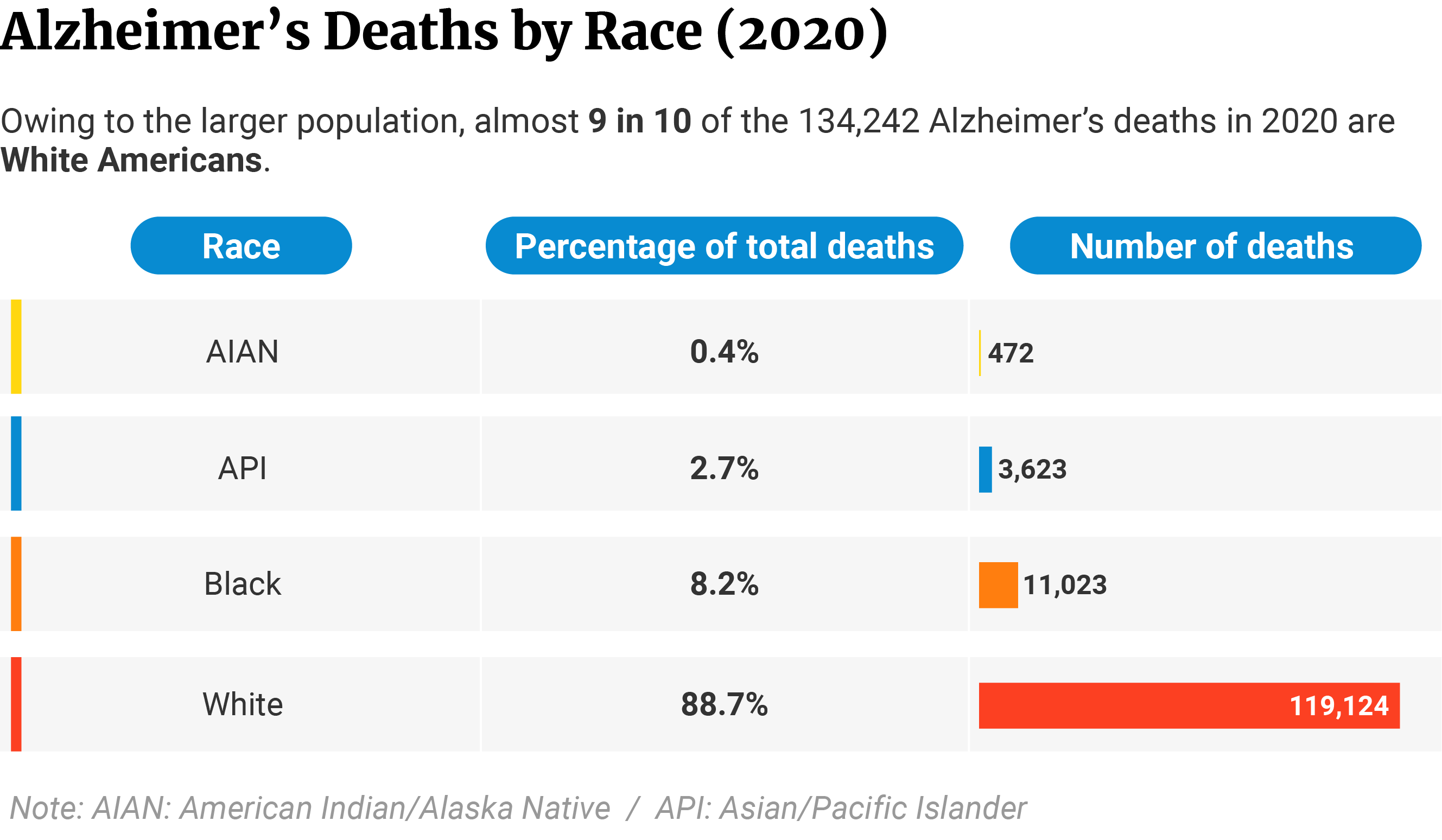
Alzheimer’s Death by Race Statistics
Of the 134,242 deaths in 2020, White Americans make up 88.7% or 119,124 of the cases [10].
The second group with the highest number of deaths is Black Americans. They make up 8.2% or 11,023 of the cases [10].
Asian or Pacific Islanders make up 2.7% of the cases with 3,623 deaths [10].
American Indians or Alaska Natives make up the least at 0.4% with 472 deaths [10].
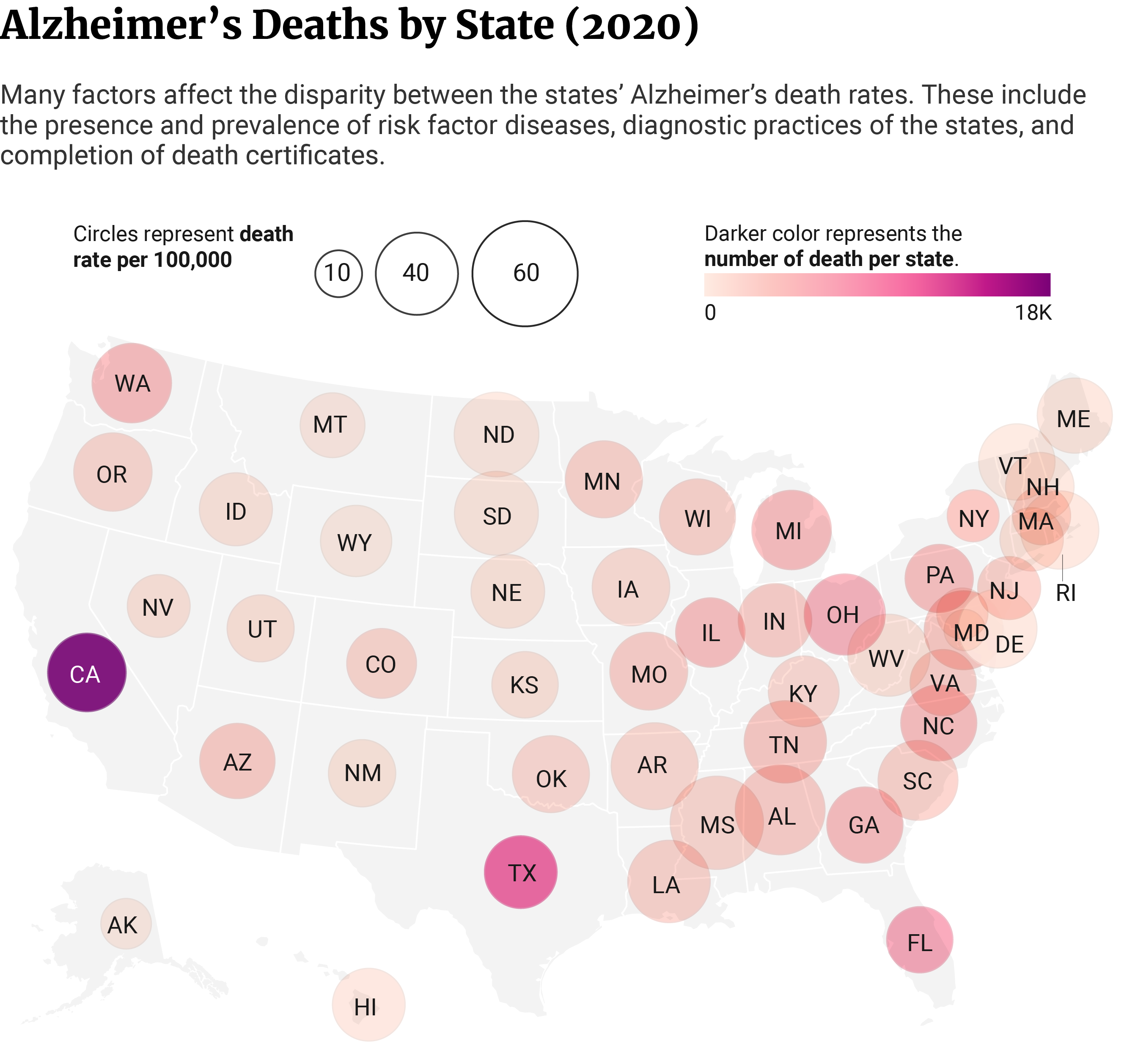
Alzheimer’s Dementia Deaths by State Statistics
California’s 18,775 Alzheimer’s deaths make up 14% of the 134,242 deaths in 2020. It’s the state with the highest number of Alzheimer’s deaths, owing to its large population [10].
Texas and Florida follow with 11,918 and 7,274 deaths, respectively [10].
The state with the lowest number of Alzheimer’s deaths is Alaska with 139 deaths. Wyoming with 227 and Vermont with 280 follow in second and third places [10].
However, when you look at the crude death rate, Mississippi has the highest with 68 per 1000,000 people [10].
Alabama has the second-highest crude death rate at 62.8 per 100,000. Arkansas comes in third place at 58.8 per 100,000 people [10].
The states with the lowest crude death rates are Alaska at 19, Maryland at 19.4, and New York at 20 per 100,000 people [10].
Annual Cost of Alzheimer’s Care in the US
Alzheimer’s disease will cost the US $321 billion in 2022 [4].
45.48% will go to Medicare at $146 billion. Medicaid will amount to 18.69% of the total cost with $60 billion [4].
25.23% or $81 billion will go to out-of-pocket expenses, while 10.59% or $34 billion will go to other expenses [4].
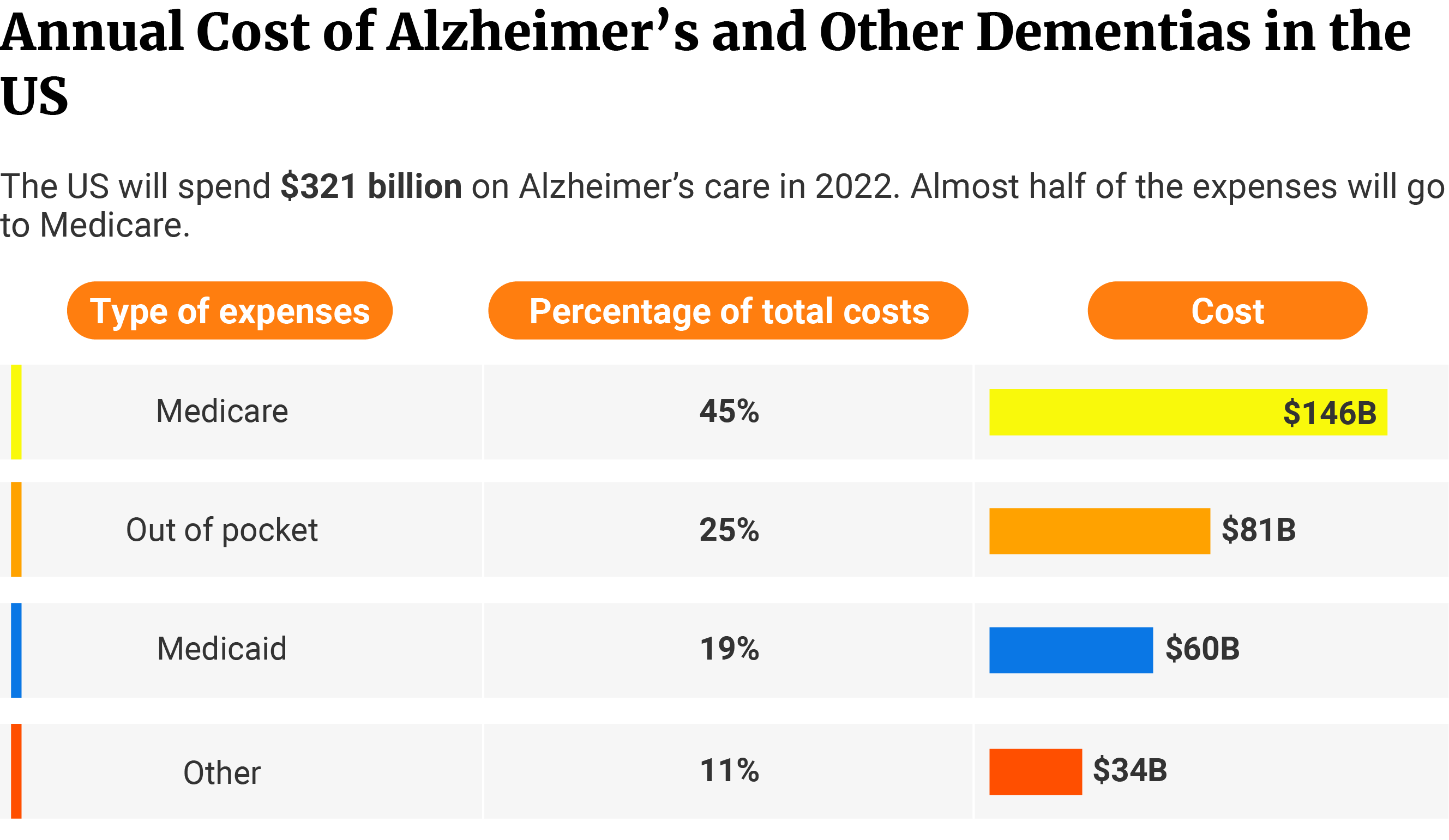
This doesn’t include unpaid care provided by family and friends. Unpaid caregiving expenses can amount to as high as $271.6 billion [4].
By 2050, the economic impact of Alzheimer’s disease could cost the US a little under $1 trillion [4].
Lifetime and Annual Cost of Alzheimer’s Care Per Patient in the US
The lifetime cost of care per patient with dementia amounted to $377,621 in 2021 [4].
Among Medicare beneficiaries, Black Americans spend the most on annual individual payments (unadjusted). White Americans spend the least on Medicare payments.
Black Americans pay 24.7% more than White Americans at $26,611 versus $21,341, respectively. Hispanics pay 15.4% higher than White Americans at $24,617 [4].
On individual monetary costs, White Americans spend the most on hospice care at $3,979. Hispanics, on the other hand, pay the highest for home healthcare at $2,281 [4].
But across the board, it’s the Black Americans who have the highest individual payments, compared to other races.
Black Americans pay 55.5% more on hospital care at $8,404, compared to White Americans at $5,404. Hispanics spend 35.3% higher than White Americans at $7,312 [4].
The same trend can be seen in physician care and skilled nursing care costs.
White Americans spend $3,666 on physician care. Black Americans spend 21.6% more at $4,457 and Hispanics 15.4% more at $4,230 [4].
As for skilled nursing care, White Americans pay $3,007 annually. Black Americans pay 31.6% and Hispanics 14.1% more at $3,957 and $3,432, respectively [4].
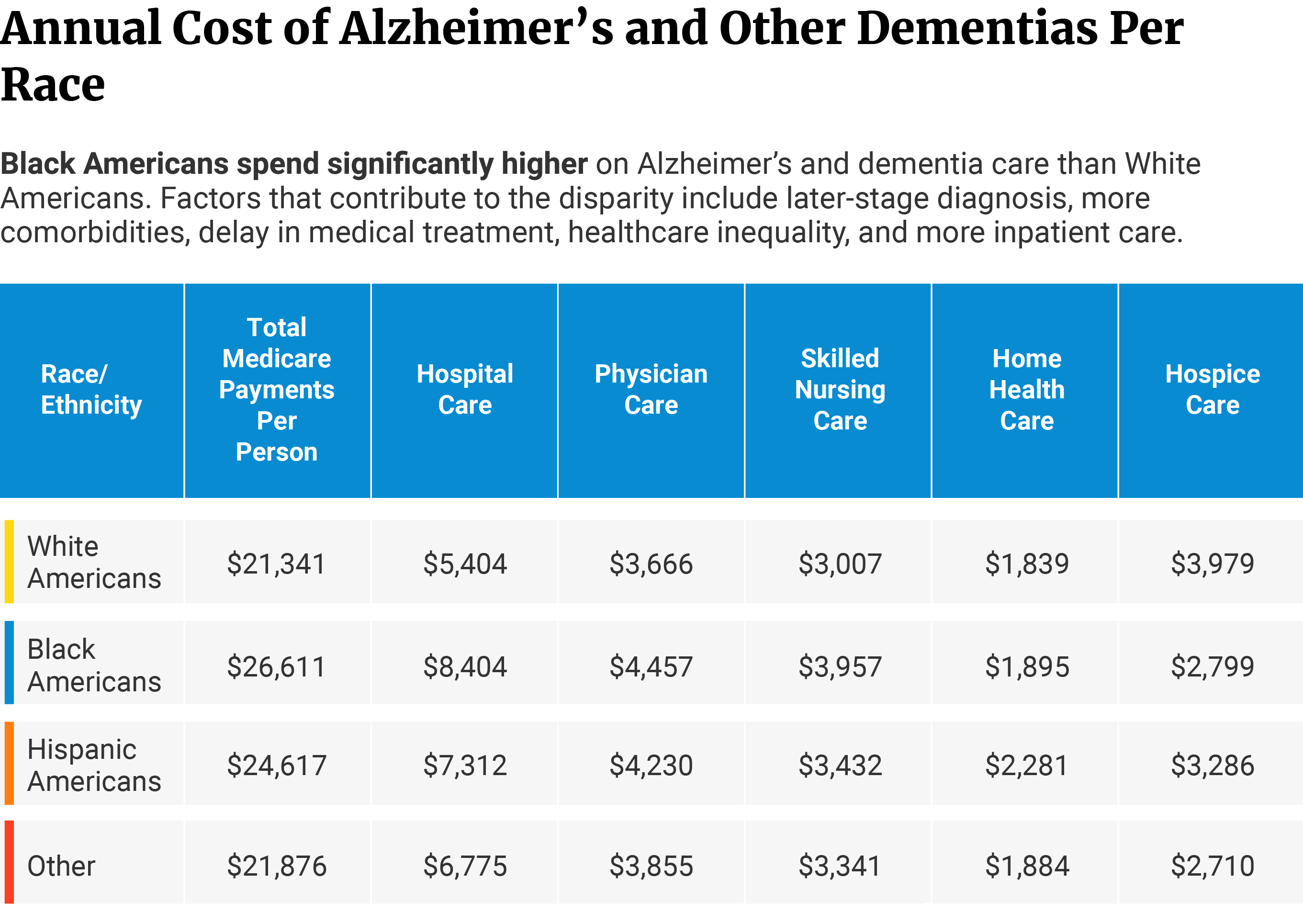
From diagnosis to death, Black Americans have a 41% higher spending rate than Whites. They shell out an additional $57,606 for Medicare costs [21].
How is Alzheimer’s Disease Treated — Common Treatments for Alzheimer’s
Alzheimer’s disease has no known cure. We only have medications to delay disease progression and improve symptoms.
1. Donepezil for Alzheimer’s Disease
In a study of 186 dementia cases, nearly 80% or 148 of them either exhibited improvement or at least remained stable. 17% showed worsened symptoms [16].
Of the 80%, 54% reported improvement in their condition, while 25% remained stable [16].
After three months, 70% of those who had donepezil showed improvement in quality of life [16].
Donepezil also helped delay placement in nursing homes. Two studies showed that [16].
- Only 1% of patients who had donepezil were placed in a nursing home within two years after joining the study. Of the untreated patients, 16% of them were placed in a nursing home.
- After three years, 11% of the donepezil-treated patients entered nursing homes. Of those who didn’t receive donepezil, 50% of them were already in nursing homes.
Donepezil helps improve acetylcholine levels in the brain. This allows for better communication between more neurons, reducing Alzheimer’s symptoms.
2. Galantamine for Alzheimer’s Disease
In a study of 119 patients, 17.6% or 21 patients maintained good cognitive functions. It also included those who remained at baseline after three years of galantamine [23].
Of the 17.6%, more than 50% of them even showed better cognitive functions than their untreated peers [23].
Galantamine also prevents the degradation of acetylcholine. It’s a neurotransmitter vital for thought and memory functions.
3. Memantine for Alzheimer’s Disease
In a study, 76% of patients with Alzheimer’s treated with memantine showed improvement in their symptoms. Of those in the placebo group, 44.7% showed improvement [25].
65.3% of those on memantine also maintained or showed improvements in BGP score. Of those who received placebo, only 39.5% were considered responders [25].
High glutamate levels produce neurotoxic effects. Memantine prevents glutamate from binding to its receptor, reducing symptoms.
BGP or Behavioral Rating Scale in Geriatric Patients measures cognitive functions. It also measures activities of daily living, mobility, and behavioral symptoms.
4. Rivastigmine for Alzheimer’s Disease
Patients taking rivastigmine have 47% higher odds of improvement in overall functions. However, they also have 116% higher odds of developing negative side effects [9].
Rivastigmine also helps increase acetylcholine levels in the brain. Neurons use this neurotransmitter for better communication.
5. Cannabinoid-Based Medicine (CBM) Including CBD for Alzheimer’s Disease
An observational study tracked 10 female patients with severe dementia. Results showed that cannabinoid-based medicine helps in managing behavioral symptoms by 40%. CBM also reduced muscle rigidity by 50% [27].
Related: Does CBD Help With Alzheimer’s Disease?
Cannabinoids work on the endocannabinoid system and other non-cannabinoid receptors in reducing symptoms.
Summary — Alzheimer’s Disease Facts and Statistics
Every 65 seconds, one individual in the US developed Alzheimer’s disease. This neurological disorder currently affects 10.7% (6.5 million) of the American population. Without medical advancements to delay disease progression, the total number of people with Alzheimer’s can increase to 13.8 million by 2060.
Medications help delay the progression of Alzheimer’s disease. But catching pneumonia increases the patient’s risk of dying by 200%. They’re most vulnerable during the 7th stage. It’s the stage where cognitive and motor functions become severely affected.
If you think a loved one may be suffering from Alzheimer’s disease, know that you can get them help and the right treatment. You can call Alzheimer’s Association’s 24/7 hotline at 800-272-3900 for health care. You may also visit their website at alz.org to know more about the clinical trials they may be offering.
References
- 7 Clinical Stages of Alzheimer’s. (2020). The Fisher Center for Alzheimer’s Research Foundation. [1]
- 7 Stages of Alzheimer’s. (2014). The Fisher Center for Alzheimer’s Research Foundation. [2]
- 2021 Alzheimer’s disease facts and figures. (2021). Alzheimer’s & Dementia, 17(3), 327–406. [3]
- 2022 Alzheimer’s disease facts and figures. (2022). Alzheimer’s & Dementia, 18(4), 700–789. [4]
- Alzheimer’s Association. (2021). Special Report: Race, Ethnicity and Alzheimer’s in America. Alzheimer’s & Dementia, 17(3). [5]
- Alzheimer’s Association. (2022). Alzheimer’s Disease Facts and Figures. Alzheimer’s & Dementia. [6]
- Alzheimer’s stages: How the disease progresses. (2021). Mayo Clinic. [7]
- Anstey, K. J., von Sanden, C., Salim, A., & O’Kearney, R. (2007). Smoking as a Risk Factor for Dementia and Cognitive Decline: A Meta-Analysis of Prospective Studies. American Journal of Epidemiology, 166(4), 367–378. [8]
- Birks, J. S., Chong, L. Y., & Evans, J. G. (2015). Rivastigmine for Alzheimer’s disease. Cochrane Database of Systematic Reviews. [9]
- CDC Wonder. (2022). Centers for Disease Control and Prevention. [10]
- Coogan, P., Schon, K., Li, S., Cozier, Y., Bethea, T., & Rosenberg, L. (2020). Experiences of racism and subjective cognitive function in African American women. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 12(1). [11]
- Dementia. (2022). World Health Organization. [12]
- Elflein, J. (2021). Leading ten causes of death in the world 2019. Statista. [13]
- Epidemiology of Vascular Dementia. (2019). Arteriosclerosis, Thrombosis, and Vascular Biology, 39(8), 1542–1549. [14]
- Gauthier, S., Webster, C., Servaes, S., Morais, J. A., & Rosa-Neto, P. (2022). World Alzheimer Report 2022: Life after diagnosis: Navigating treatment, care and support. Alzheimer’s Disease International. [15]
- Knowles, J. (2006). Donepezil in Alzheimer’s disease: an evidence-based review of its impact on clinical and economic outcomes. Core Evidence, 1(3), 195–219. [16]
- Lennon, J. C., Aita, S. L., Bene, V. A. D., Rhoads, T., Resch, Z. J., Eloi, J. M., & Walker, K. A. (2021). Black and White individuals differ in dementia prevalence, risk factors, and symptomatic presentation. Alzheimer’s & Dementia, 18(8), 1461–1471. [17]
- Life Expectancy Following Diagnosis Of Alzheimer’s Disease Depends On Age At Diagnosis. (2002). Johns Hopkins. [18]
- Manabe, T., Fujikura, Y., Mizukami, K., Akatsu, H., & Kudo, K. (2019). Pneumonia-associated death in patients with dementia: A systematic review and meta-analysis. PLoS One, 14(3), e0213825. [19]
- National Institute on Aging. (2019). What Causes Alzheimer’s Disease? National Institutes of Health. [20]
- Ornstein, K. A., Zhu, C. W., Bollens-Lund, E., Aldridge, M. D., Andrews, H., Schupf, N., & Stern, Y. (2018). Medicare Expenditures and Health Care Utilization in a Multiethnic Community-based Population With Dementia From Incidence to Death. Alzheimer Disease & Associated Disorders, 32(4), 320–325. [21]
- Rajan, K. B., Weuve, J., Barnes, L. L., McAninch, E. A., Wilson, R. S., & Evans, D. A. (2021). Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimer’s & Dementia, 17(12), 1966–1975. [22]
- Raskind, M. A., Peskind, E. R., Truyen, L., Kershaw, P., & Damaraju, C. V. (2004). The Cognitive Benefits of Galantamine Are Sustained for at Least 36 Months: A Long-term Extension Trial. Archives of Neurology, 61(2), 252–256. [23]
- Smoking increases risk of dementia. (2014). Alzheimer’s Disease International. [24]
- Tampi, R. R., & van Dyck, C. H. (2007). Memantine: efficacy and safety in mild-to-severe Alzheimer’s disease. Neuropsychiatric Disease and Treatment, 3(2), 245–258. [25]
- Tejada-Vera, B. (2013). Mortality from Alzheimer’s disease in the United States: Data for 2000 and 2010. In Centers for Disease Control and Prevention (NCHS data brief, no 116). National Center for Health Statistics. [26]
- Timler, A., Bulsara, C., Bulsara, M., Vickery, A., Smith, J., & Codde, J. (2020). Use of cannabinoid-based medicine among older residential care recipients diagnosed with dementia: study protocol for a double-blind randomised crossover trial. Trials, 21, 188. [27]
- Tom, S. E., Hubbard, R. A., Crane, P. K., Haneuse, S. J., Bowen, J., McCormick, W. C., McCurry, S., & Larson, E. B. (2015). Characterization of Dementia and Alzheimer’s Disease in an Older Population: Updated Incidence and Life Expectancy With and Without Dementia. American Journal of Public Health, 105(2), 408–413. [28]
- Wang, L., Davis, P. B., Volkow, N. D., Berger, N. A., Kaelber, D. C., & Xu, R. (2022). Association of COVID-19 with New-Onset Alzheimer’s Disease. Journal of Alzheimer’s Disease, 89(2), 411–414. [29]
- Yegambaram, M., Manivannan, B., Beach, T., & Halden, R. (2015). Role of Environmental Contaminants in the Etiology of Alzheimer’s Disease: A Review. Current Alzheimer Research, 12(2), 116–146. [30]
- Zhang, Q., Schultz, J. L., Aldridge, G. M., Simmering, J. E., Kim, Y., Ogilvie, A. C., & Narayanan, N. S. (2021). COVID-19 Case Fatality and Alzheimer’s Disease. Journal of Alzheimer’s Disease, 84(4), 1447–1452. [31]